Case Vignette
Multiple Injuries In The Lumbar Spine
The AMA 5 Guides recommend that expert reporters quantifying impairments use the so-called “Diagnosis Related Estimate Category” method for assessment. There are several reasons for that recommendation. One relates to the potential for unreliability when assessing ranges of motion of the lumbar spine. The assessor may be mistaken or alternatively, the patient may be inconsistent and/or even overreactive. The use of the Diagnosis Related Estimate Category system assists in levelling the playground for assessment.
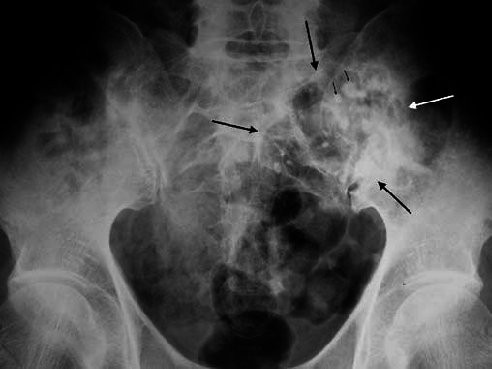
The Guides however are equally specific in their advice concerning multiple injuries in the same vertebral column segment. That is to say, if there are two or more discrete injuries in the lumbar spine, it is not the Diagnosis Related Estimate Category that should be used but rather, the Range of Motion method. For example, if there is a fracture of the transverse process, a fracture of a vertebral body at L3 and a fracture of a lamina at L5, it is the Range of Motion method that should be used.

There are two steps to the Range of Motion analysis. The first relates to measuring the losses as a result of the specific fractures according to Table 15-7. There are separate sections within that Table that make reference to fractures of posterior elements, a vertebral body, disc lesions or forward slippage of one vertebral body on the other (spondylolisthesis).

In addition to quantifying the loss related to the two or more discrete injuries in that lumbar spine, the reporter must also measure the ranges of motion in the sagittal and coronal planes. Rotation should also be measured, especially in the thoracic spine.
The losses measurable using Table 15-7 and the losses measurable related to the restrictions in range of motion are then combined using appropriate Combined Values Tables to yield a final functional whole person impairment.
This can lead to confusion amongst reporters. It is confusion that causes disagreement and usually, it is disagreement that compounds the processes of mediation and Court trials.

It is most useful for all involved if your expert reporter is not only familiar with disorders of the vertebral column, but also the proper use of the AMA 5 Guides.