CASE VIGNETTE – FEBRUARY 2020
Indolent Infection Following Serious Orthopaedic Injuries
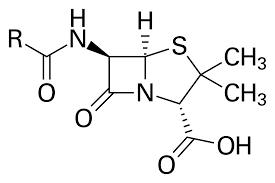
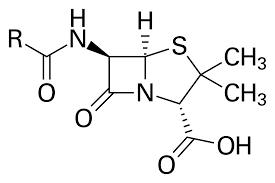
Bacterial infections continue to give rise to significant difficulties with orthopaedic surgery, whether it be in the emergency setting or at the time of elective operations. The pivotal work of Fleming and Florey bringing penicillin to market in the first two or three decades of the last century made a significant change to the outcome of surgical endeavours. Research and development by the major drug marketing companies has brought a plethora of new and different types of antibiotics into the market.
Unfortunately, our bacterial adversaries are extremely clever in the way they mutate and learn to overcome the obstacles presented by the antibiotics, and thereby thrive in the post-surgical setting. Some of the difficulty is of our own doing. There are practitioners who will use antibiotics unwisely, patients who do not always take a full course, and bacterial whose virulence sets them apart in their ability to develop resistance.
So serious is this problem that as we enter the next decade, it is likely that we will witness infections even in our own community with bacteria expressing resistance to every chemotherapeutic agent at our disposal.
Most infections are obvious. They are accompanied by pain, redness, swelling, an increase in temperature and often a discharge (whether it be serous or pus). Other infections however are vastly more subtle and can remain indolent for weeks, months and even years.

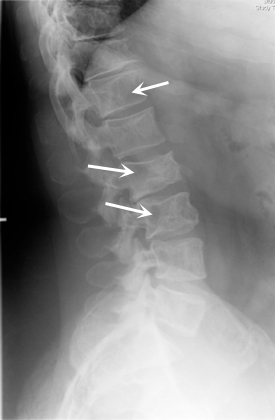
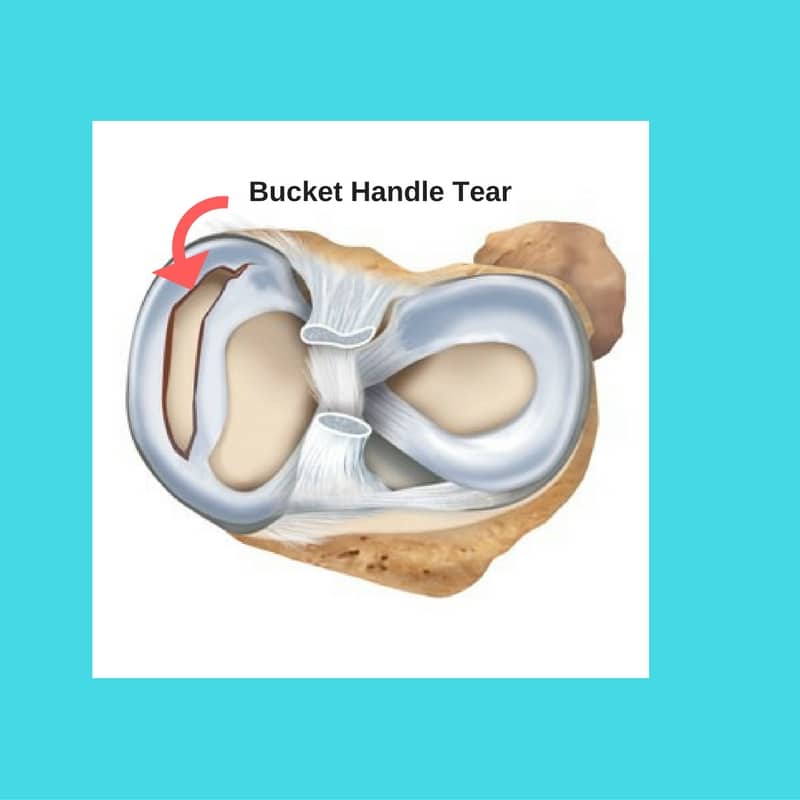
For example, it is possible to have an osteomyelitic bacterium that has lay quiescent in sequestrum in a bone for some decades. It is only when that sequestrum or local deposit is disturbed (say at the time of an injury with a fracture or at the time of undergoing a hip or knee replacement) that the bacterium is again released, prodded into action and a spectacular infectious result is witnessed.
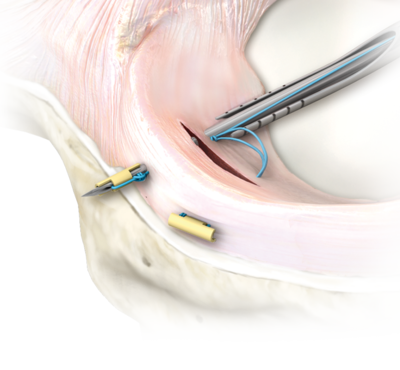
Whilst non-operative modalities such as the use of antibiotics are of great importance in fighting infections, it is the scalpel which is the most effective of all tools. Abscesses should be drained, dead and devitalised tissue debrided or removed and vascularisation of the local region maximised.

This has very special medicolegal implications. There is a risk that a patient may be deemed to have achieved the state of Maximal Medical Improvement. The condition could be thought to be both stable and stationary. A claim could therefore be closed prematurely. The recurrence of an indolent infection after claim closure could result in significant morbidity, great financial imposts and even mortality. It is worthwhile ensuring that your medicolegal expert always considers this possibility when formulating a report.